Discharge Charting Example
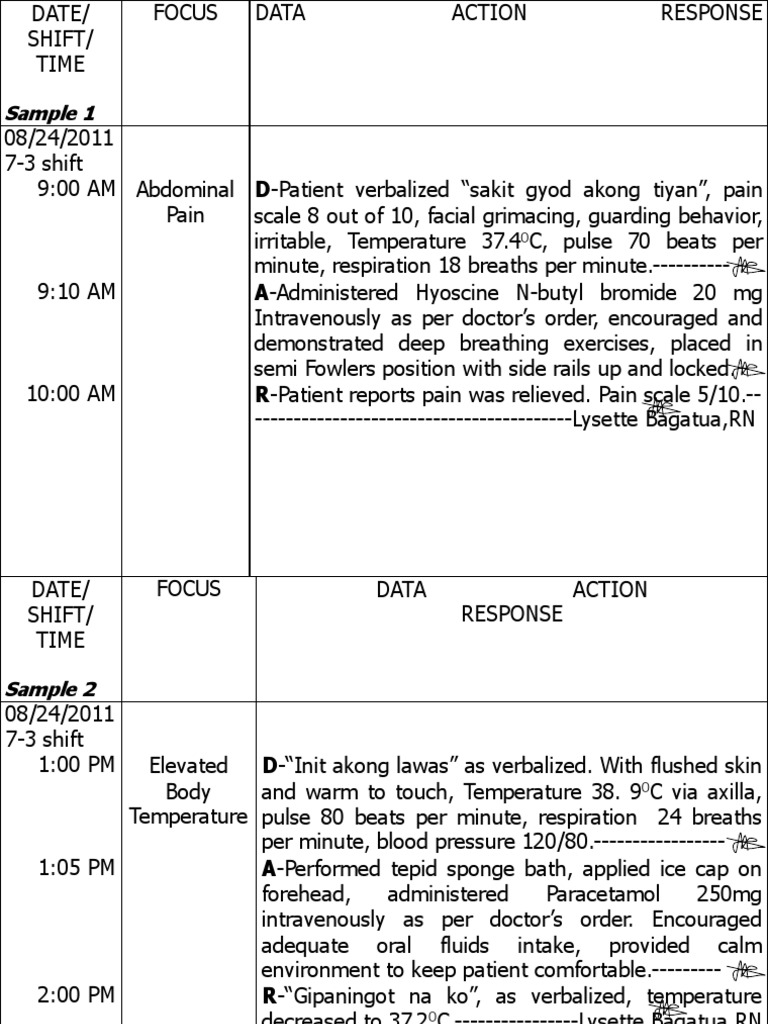
Discharge Charting Example - In these charts, nurses can monitor patient data and evaluate their. Web nursing progress charts include nursing progress notes and other vital information relevant to the patient’s status from admission until discharge. The nursing progress chart may. How do you use the discharge planning checklist template? The discharge planning checklist template. Web common formats used to document patient care include charting by exception, focused dar notes, narrative notes, soapie progress notes, patient discharge summaries, and. Define roles and standardize documentation. Use our template to ensure a smooth termination process and maintain a positive. You can incorporate elements of the. Smith is director and associate professor in the associate degree. Use our template to ensure a smooth termination process and maintain a positive. They're commonly combined with patient discharge instruction forms and provide useful. Web the nursing discharge note documents all pertinent information about a patient's hospital stay, including their diagnosis, treatment, condition at discharge, discharge instructions,. The nursing progress chart may. Web updated july 28, 2023. Web the ideal discharge planning strategy focuses on engaging the patient and family in the discharge process from the hospital to home. In these charts, nurses can monitor patient data and evaluate their. Educate the patient and family in plain language about the. Medical care given to patients must be recorded appropriately. You can incorporate elements of the. Educate the patient and family in plain language about the. Web discharge planning involves a coordinated effort between the patient/resident, caregiving professionals, family members, and community supports. In these charts, nurses can monitor patient data and evaluate their. Use our template to ensure a smooth termination process and maintain a positive. The discharge planning checklist template. Web common formats used to document patient care include charting by exception, focused dar notes, narrative notes, soapie progress notes, patient discharge summaries, and. Length 4 cm, width 3 cm, depth 2 mm. Here are the discharge summary templates. Web updated july 28, 2023. Web download template download example pdf. Define roles and standardize documentation. Educate the patient and family in plain language about the. Web discharge summaries reflect the reassessment and evaluation of your nursing care. Web download template download example pdf. In these charts, nurses can monitor patient data and evaluate their. Use our template to ensure a smooth termination process and maintain a positive. Web a discharge summary example is an official document and as such, might jeopardize the care if the doctor makes any errors while making it. Here are the discharge summary templates. As mentioned, a patient discharge form contains key information essential for. Medical care given to patients. They're commonly combined with patient discharge instruction forms and provide useful. Web learn what a discharge note or discharge summary is for terminating therapy with your client. The discharge planning checklist template. Web discharge planning involves a coordinated effort between the patient/resident, caregiving professionals, family members, and community supports. You can incorporate elements of the. The discharge planning checklist template. Web upon discharge or transfer ; Web for example, if a patient returns to a hospital months after initial treatment, documentation of the patient’s symptoms and treatments can inform current diagnoses. Web updated july 28, 2023. Smith is director and associate professor in the associate degree. Use our template to ensure a smooth termination process and maintain a positive. Web download template download example pdf. You can incorporate elements of the. Assess the patient's medical condition, functional abilities, and support systems, and establish recovery goals. In these charts, nurses can monitor patient data and evaluate their. The nursing progress chart may. In these charts, nurses can monitor patient data and evaluate their. You can incorporate elements of the. Web download template download example pdf. Here are the discharge summary templates. They're commonly combined with patient discharge instruction forms and provide useful. As mentioned, a patient discharge form contains key information essential for. Here are the discharge summary templates. Assess the patient's medical condition, functional abilities, and support systems, and establish recovery goals. Web charting is a nursing process that includes all the documentation required from nurses. Web discharge summaries reflect the reassessment and evaluation of your nursing care. Web learn what a discharge note or discharge summary is for terminating therapy with your client. Define roles and standardize documentation. What should be in a patient discharge form? Length 4 cm, width 3 cm, depth 2 mm. Web common formats used to document patient care include charting by exception, focused dar notes, narrative notes, soapie progress notes, patient discharge summaries, and. Web upon discharge or transfer ; Highlight warning signs and problems. The discharge planning checklist template. You can incorporate elements of the. How do you use the discharge planning checklist template?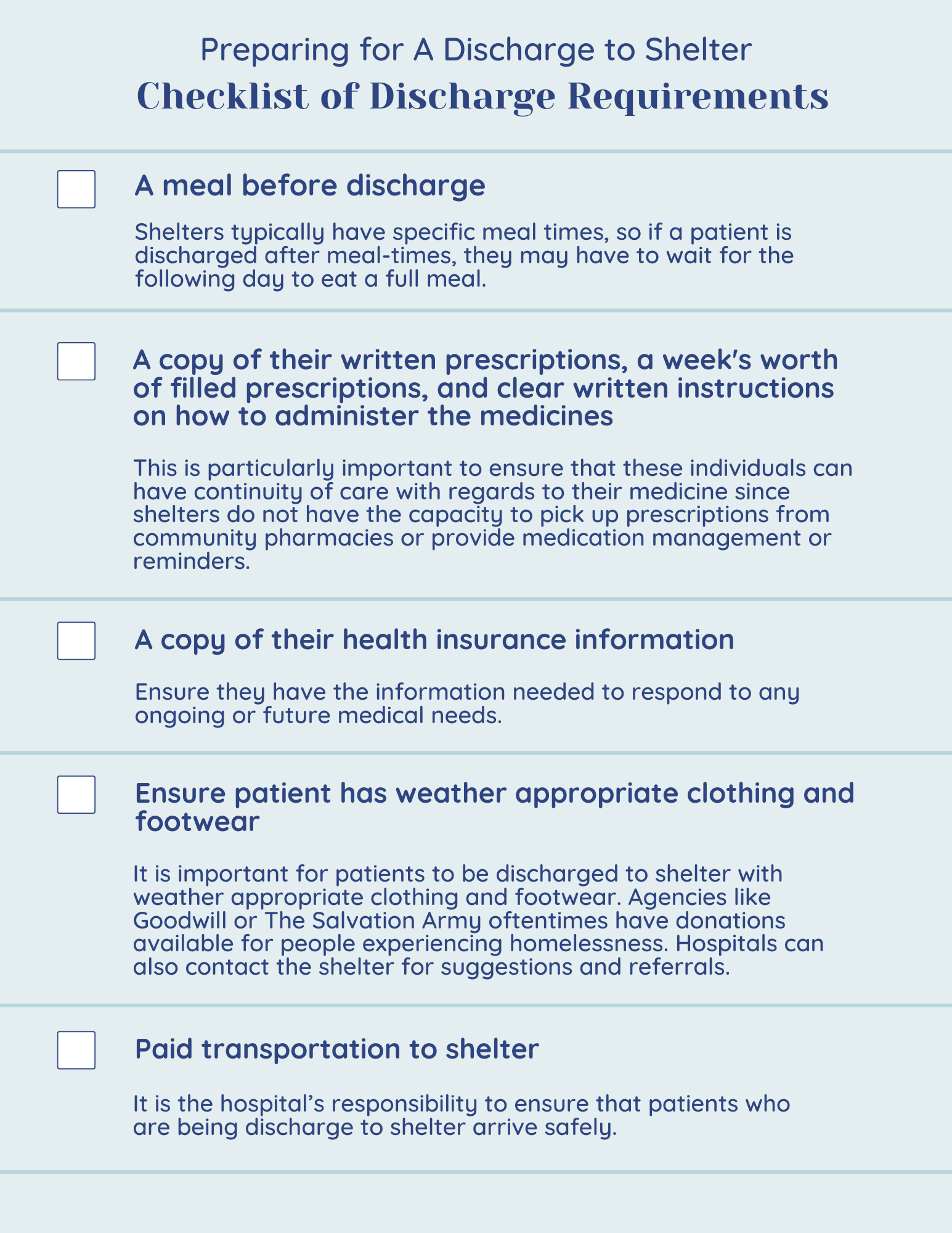
Discharge Planning Skills and Resources Mass.gov
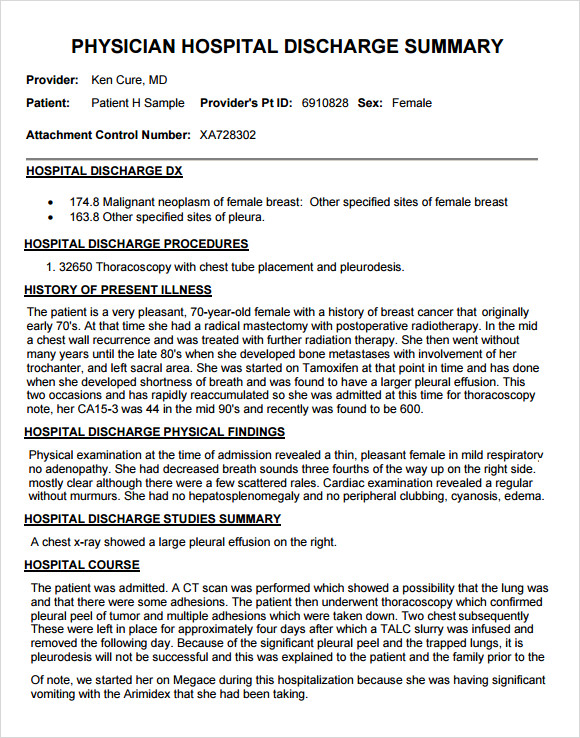
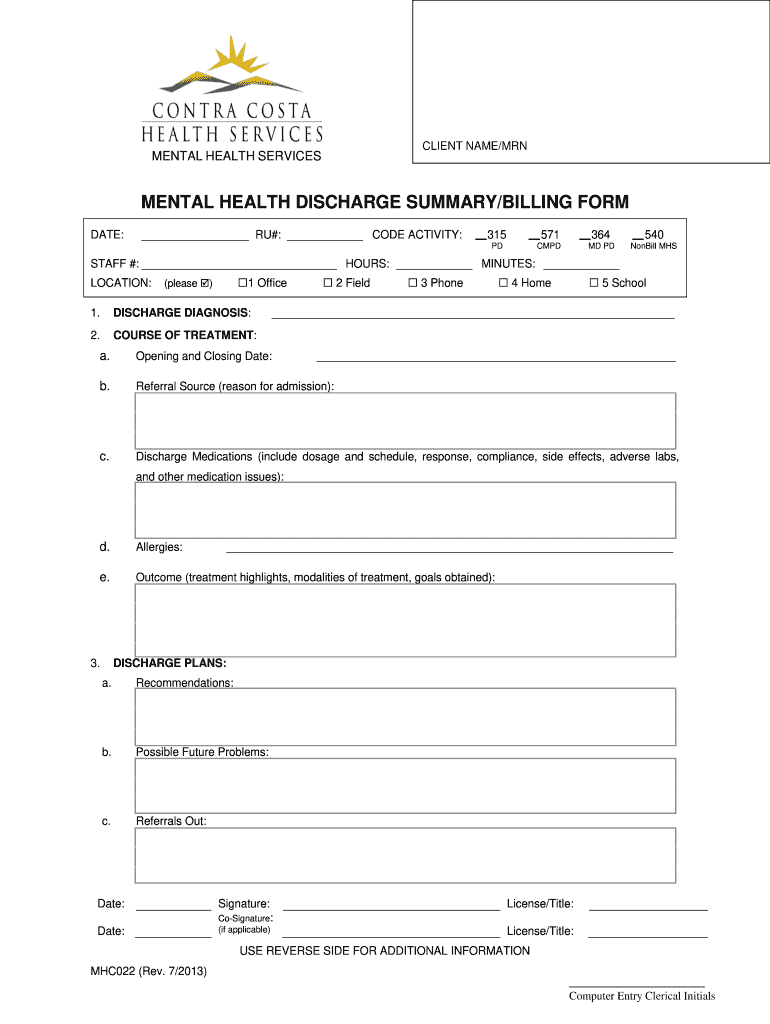
FREE 7+ Sample Discharge Summary Templates in PDF MS Word
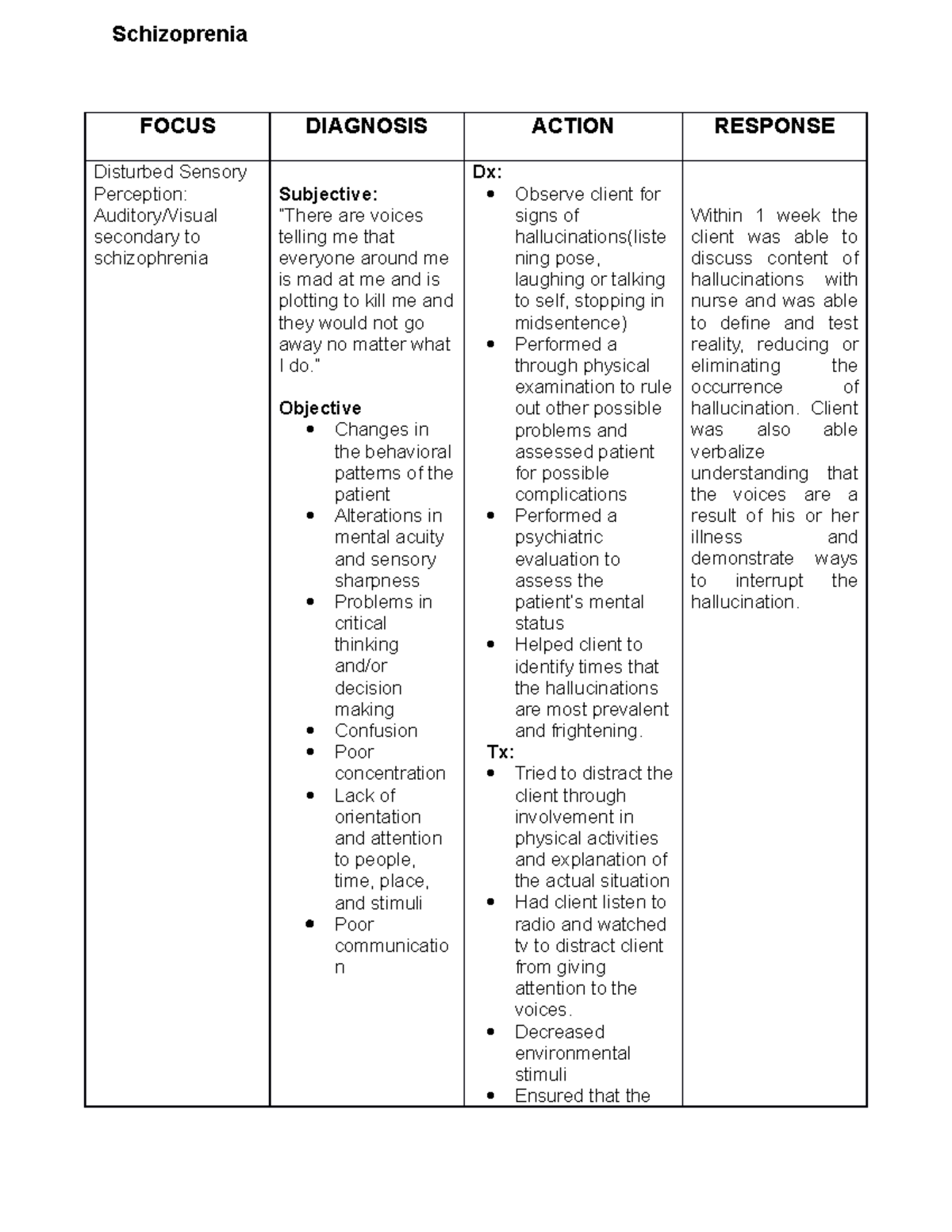
FDAR or Nursing Care Plan FOCUS DIAGNOSIS ACTION RESPONSE Disturbed
Fdar Samples Presentation Surgery Intravenous Therapy
Fdar Charting and Discharge Planning PDF Relaxation (Psychology
Sample Discharge Plan
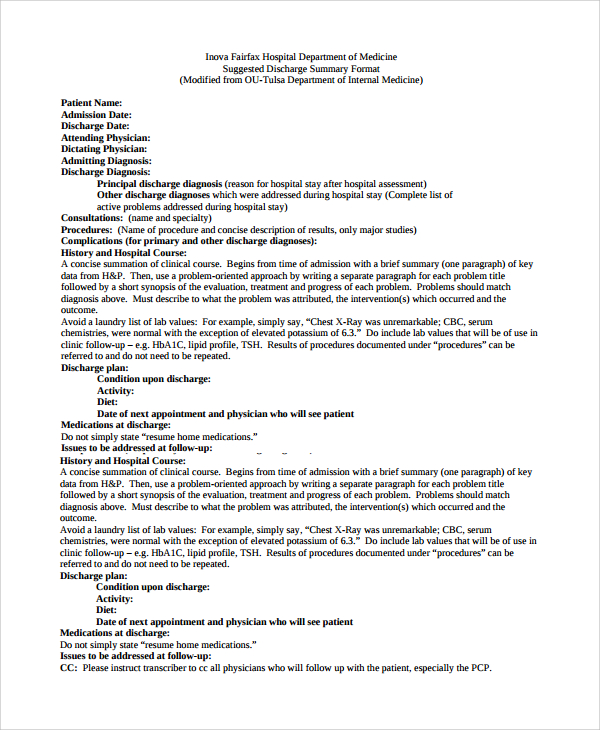
14+ Discharge Summary Samples Sample Templates
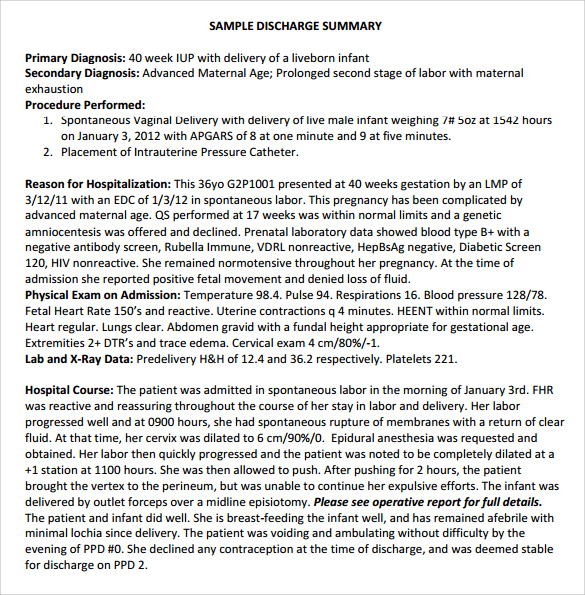
FREE 11+ Sample Discharge Summary Templates in PDF MS Word
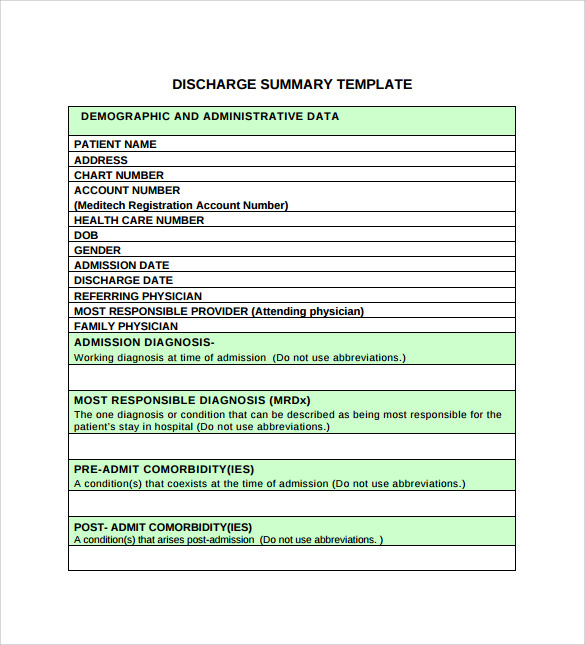
11+ Discharge Summary Samples Sample Templates
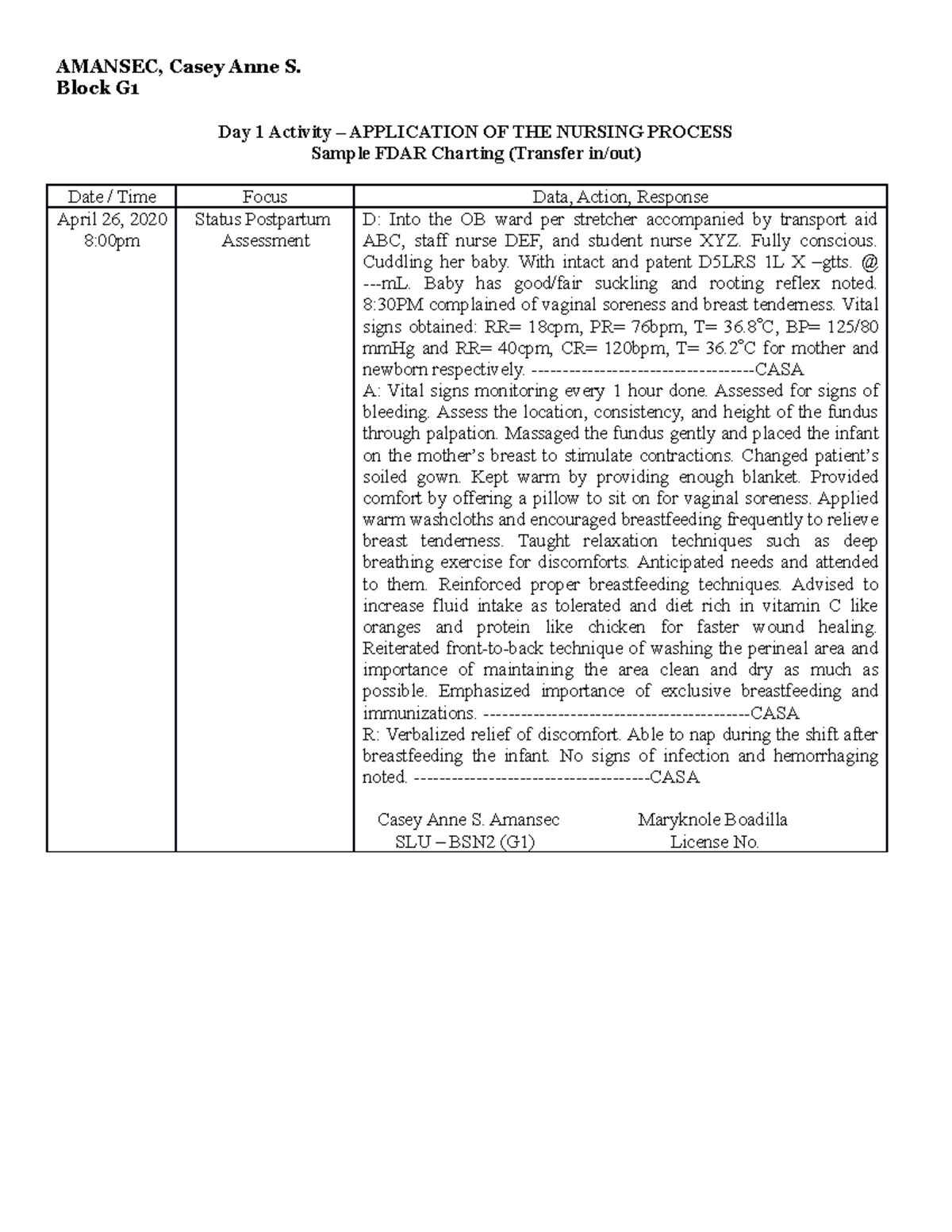
Fdar Charting Sample
Web Nursing Progress Charts Include Nursing Progress Notes And Other Vital Information Relevant To The Patient’s Status From Admission Until Discharge.
Web Download Template Download Example Pdf.
Web For Example, If A Patient Returns To A Hospital Months After Initial Treatment, Documentation Of The Patient’s Symptoms And Treatments Can Inform Current Diagnoses.
Smith Is Director And Associate Professor In The Associate Degree.
Related Post: